With the novel coronavirus (COVID-19) ripping through American jails and prisons, concern is growing over the mental health of prisoners rendered powerless amid a highly contagious and deadly pandemic.
As we've previously reported, mental illness helps fuel incarceration in the United States, which has the highest incarceration rate in the world.
The three largest jails in the country hold more patients suffering from mental illness than do psychiatric facilities. Meanwhile, there are far more people incarcerated with a serious mental illness than receiving treatment in a dedicated facility.
In an interview for a previous podcast episode, Leah Pope, senior research fellow at the Vera Institute for Justice, explained of the mentally ill: They are "overrepresented at all stages in the criminal justice system."
“I think it’s become a common refrain that our jails are our de facto mental health institutions in this country,” she said. “And it’s definitely true because you go into any jail and you’re more likely to find someone with mental illness than you are in the community. I think the criminalization of mental illness has a lot of underpinnings.”
Now the question is, what impact will the pandemic have on incarcerated people? Already, nearly 1,000 people locked up in jails and prisons have died from the disease. Correctional facilities have some of the largest infection rates in the country, despite warnings early in the pandemic that the virus could spread uncontrollably in these institutions.
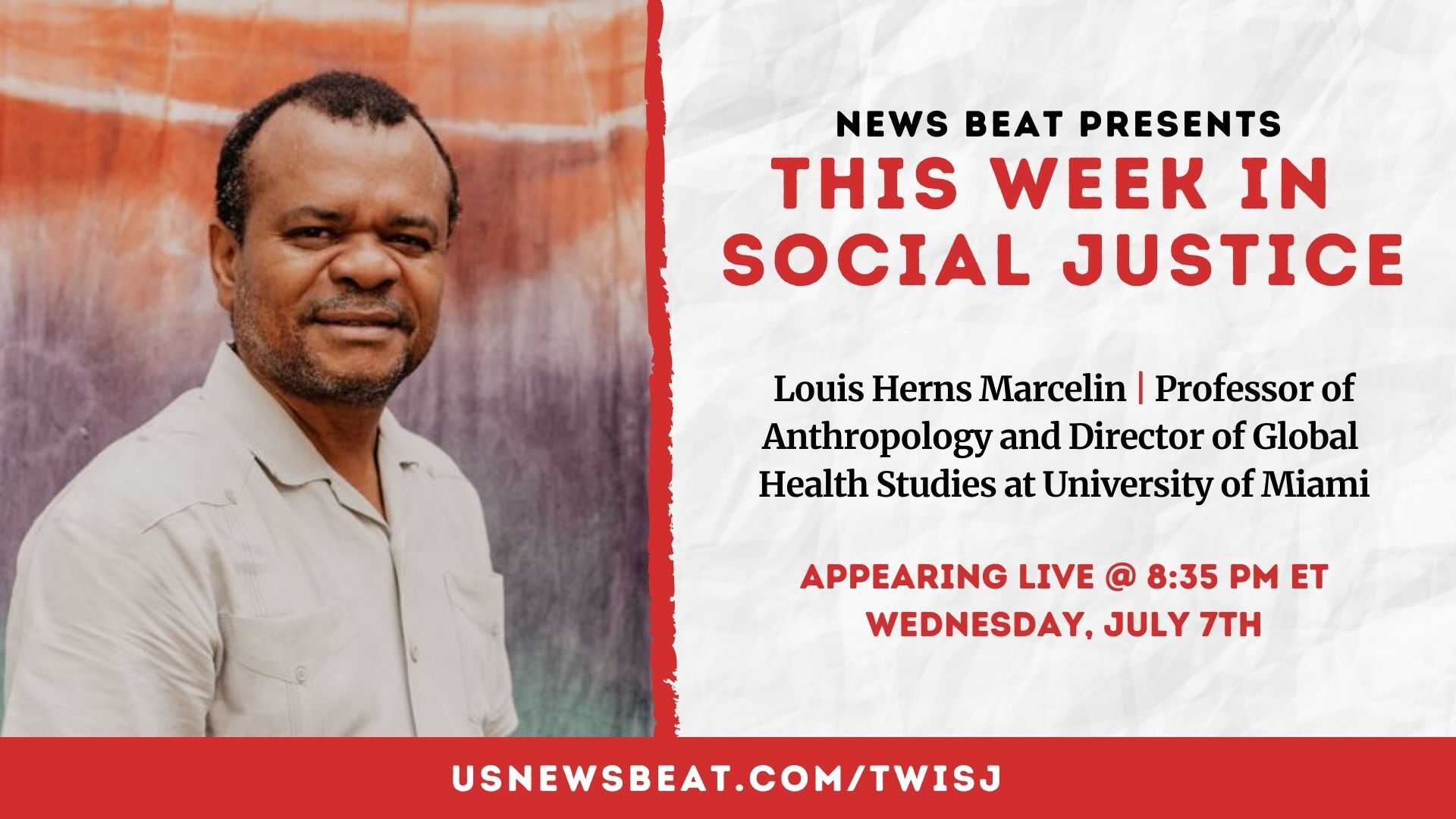
In an episode released on Aug. 28, News Beat revisited the issue of COVID-19 and incarceration. One of our guests on that episode, Sharon Dolovich, faculty director of the UCLA Prison Law & Policy Program who oversees the university's COVID-19 jail and prison data collection project, shared her concern about the mental health impact for those imprisoned.
Here's a transcript of this portion of our interview with Dolovich, edited for clarity.
"When a person goes into lock down, what happens is people are required to stay in their cells and their dorms. There's no movement. There's no programming. There's no visits. Basically, your life stops. And I'll say that when that happens, in general, people who wrestle with mental health issues can decompensate, because the kinds of things that help them maintain their equilibrium are no longer there. And the kind of mental health that's available in most commercial facilities is minimal, at best. So now, think about what that would be like—let's say you have suicidal tendencies, you have high anxiety or you suffer from serious depression. And you are now in a situation where you're in a prison, where there's no movement, you've been locked down since March, and you're afraid because you know that there's this pandemic. And you know that because of your living experience, that you're crowded in congregate settings where you can't socially distance, and you can't really protect yourself. And maybe you don't have access to soap and water to wash your hands. And you live and sleep and breathe within inches of other people.
"So you know you're at great risk of getting the virus and you probably aren't getting great information from the prison in general, and you're probably seeing insufficient efforts by the people who run the facility to actually keep people safe. I mean, what we're seeing is, rather than making real efforts to figure out how to keep people safe in prison, you have prison officials who are fighting legal actions to try to improve conditions on the inside to reduce suffering of the virus. So you're not you're not just outside fighting for the people who are in custody, you're one of those people, and all the things that would trigger your desperation are in place.
"So, not a lot of people have been talking about this issue because the focus has been on the physical impact of the virus. But I've been thinking for a while that we are likely to be seeing an increase in the number of suicides among people in custody. And there was a case that was just in The New York Times yesterday of a man in a prison in Connecticut who hanged himself with the mask that had been given to them to protect themselves against COVID. I think that some of the response to that suicide has been from prison officials saying, 'Well, that's the reason we shouldn't give people masks,' but actually, we should be giving people masks, because that's what they need to keep them safe. What we should be doing is trying to arrange experience of custody in a way that doesn't deeply exacerbate the kinds of triggers that people with mental health issues experience. And that should include identifying those people who are particularly at risk of mental health crises in prison and getting them out, finding some other way to provide them treatment that doesn't put them at risk."